How is Lynch syndrome diagnosed? Do I have an inherited condition?
In the majority of cases, colorectal cancer is not an inherited condition. It is common in the general population, affecting 1 in 14 men and 1 in 19 women at some point during their life, more commonly after the age of 60. Most colorectal cancers occur sporadically or out of the blue. However, in about 5-10% (5-10 in 100) of the individuals who develop colorectal cancer is caused by a genetic alteration (a change in their genetic code instructions, or what we are going to call a ‘genetic change’). In about 3-5% (3-5 in 100) of all colorectal cancers, the genes affected are those whose task is to repair abnormalities when cells are made.
These repair genes (called DNA mismatch repair genes) protect us from developing certain cancer types. This is the case in Lynch syndrome, which is the most common inherited type of colon cancer. It affects 1 in 278 people.
It’s not straightforward to find out if a colorectal cancer is inherited or sporadic (out of the blue). To find out if someone has an inherited cancer that is being passed down in the family, there are different tests that need to be performed. In addition to taking a detailed family history, for Lynch syndrome some tests are performed in the cancer (tumour) sample. This is because Lynch syndrome leaves fingerprint in the tumour. There are 2 types of tumour tests commonly used.
Immunochemistry (IHC)
Every person diagnosed with colorectal cancer has IHC performed in their cancer. IHC looks at the expression of the proteins produced by these “mismatch repair” genes. If there is a loss of expression of any of these proteins, you may be offered genetic testing to find out if you have Lynch syndrome
Microsatellite Instability (MSI)
This is another type of genetic test on the tumour to find out if you are likely to have Lynch syndrome. If the result is positive you might have Lynch syndrome and, you will be offered genetic testing.
In some cases, additional testing is required
MLH1 promoter Hypermethylation (MLH1 Methylation)
Methylation can occur in sporadic cancers. In some cases, following IHC test, this test might be necessary to clarify if the cancer is sporadic and originates in the tumour, or it could possibly be inherited. If the result of this test shows that cancer sample is methylated, it clarifies that the cancer is sporadic and originates in the tumour. If not you will be offered genetic testing.
These tumour tests will clarify whether your cancer is likely to be inherited or sporadic. If your tumour test results show that there is a possibility that you might have Lynch syndrome, you will be offered genetic testing.
What is Lynch Syndrome?
Lynch syndrome is an inherited condition that makes people more likely to develop particular types of cancer. In order to explain Lynch syndrome, we need to explain how normal cells work and divide and, how cancer occurs.
For our body to grow and repair itself, cells must create new cells. If you cut yourself, your skin cells continue to divide until the wound is healed. Normal healthy cells know when to stop dividing. Cancer happens when cells continue dividing when they are supposed to stop. As the cancer cells grow, they begin to crowd out normal cells and eventually form a lump. A lump of cancer cells is called a tumour.
There are some mechanisms in our body that protect us against cancer. These mechanisms guard cells and make sure that the cells know when to stop dividing. When these mechanisms identify cells that are unable to stop multiplying, these mechanisms repair or remove these cells, and by doing so they prevent cancer from occurring. One of these mechanisms is created by the DNA mismatch repair genes called MLH1, MSH2, MSH6, and PMS2. Everybody have these genes. In Lynch syndrome one of these genes is not working properly, which means that their cancer protection mechanism is not working at 100%, which means that individuals with Lynch syndrome have less protection against cancer. These mismatch repair genes work like police officers in our body, checking that cells are made properly and don’t divide and multiply out of control. If these genes aren’t working properly, it might result in less police officers, which results in less protection against cancer.
This means that people living with Lynch syndrome have less protection, rather than having a genetic alteration that causes cancer itself. For this reason, not all individuals living with Lynch syndrome will develop cancer, but having less protection makes it more likely. Most people living with Lynch syndrome are well.
Lynch syndrome is caused by a genetic change in one of these DNA mismatch repair genes called MLH1, MSH2, MSH6, and PMS2. There is a fifth gene involved called EPCAM gene because it turns off the neighbouring MSH2 gene. EPCAM alterations are very rare and only account for 6% of Lynch syndrome cases.
The main concern in Lynch syndrome is colorectal cancer. For women endometrial (womb) cancer is also a concern, and to a lesser degree ovarian cancer. There is small increase in likelihood to develop few other cancer types that you may need to keep an eye on, but this will be explained later. The risk or likelihood of developing different cancer types depend on which gene is implicated, and other factors such as gender, and age. You can find your gene-specific information in the screening & risk reducing strategies section.
Having a diagnosis of Lynch syndrome can be a double edge sword. On one hand, it could be worrying to know that you have a higher likelihood to develop cancer. On the other hand, you are armed with knowledge and an enhanced screening programme that will help you prevent these cancer types and live a normal and fulfilling life. It will empower you to manage your care and reduce the risk of cancer, or catch it and treat early.
What is most important, you are not alone! As many as 1 in 280 people live with Lynch syndrome. There are over 7 billion people on earth. Over 25 million of them have Lynch syndrome, just like you.
If you would like to meet other people living with Lynch syndrome, there is association called Lynch Syndrome UK run by people living with Lynch syndrome. They have useful resources, organise events, and online as well as face-to-face support groups where you can meet people just like you. To visit their website, follow this link:
https://www.lynch-syndrome-uk.org/
How did I get Lynch syndrome?
To understand how Lynch syndrome happens, we need to understand DNA and genes. DNA is the code our bodies use to make genes. Genes are the instructions that tell our body how to grow and develop and each have their own job to perform. Some of our genes determine what hair and eye color we have, and some are responsible for protecting us against diseases like cancer.
Inherited conditions are due to a genetic change (also known as a variant or genetic alteration) in a particular gene, which can be passed on in a family. A genetic change may change the level of protection a family has against disease such as cancer.
Lynch syndrome is usually caused by a change in the mismatch repair genes. Mismatch repair genes protect us against cancer by repairing DNA mistakes that can occur when our cells are made. The Lynch syndrome genes are like police officers in our body, checking that cell know when to stop dividing and do not turn into cancer cells, and by doing so they protect us against cancer. If these genes aren’t working properly, this might result in less police officers protecting us against cancer.
When we are conceived, we inherit 2 copies of every gene, 1 copy from our mother and 1 copy from our father. If one of our parents has Lynch syndrome, at the point of conception, they have a 50% chance of passing on their altered copy and 50% chance of passing on their unaltered copy. If a person inherits the altered copy, they will have Lynch syndrome, this is also known as an autosomal dominant inheritance pattern. This also means a person with Lynch syndrome has a 50% chance of passing on their altered gene each time they have a child.
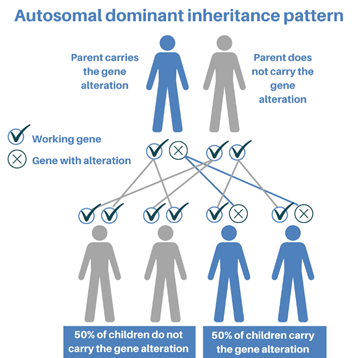
Figure created by North East Thames Regional Cancer Genetics Service
Mismatch repairs genes are inherited from your parents. If you inherit an altered copy of the gene which causes Lynch syndrome, you have Lynch syndrome. Luckily, the copy from the other parent may work just fine. However, there is a chance that, one day your working mismatch repair gene will make a mistake in one of the organs affected by Lynch syndrome. When both your mismatch repair genes are no longer working, you have less protection against cancer and so, cancer will be more likely to occur.
In 99% of the cases, you would have inherited Lynch syndrome from one of your parents. In this case, it is possible that your siblings will have it too. If you do not have Lynch syndrome, you cannot pass it on to your children because you cannot pass on something that you don’t have.
It is possible to have Lynch syndrome without inheriting it from your parents, but this is extremely rare. In this case, the genetic alteration happens by nature after conception, and you are the only one that has it. This is called a “de novo” genetic alteration. In this case your siblings and parents are unlikely to have Lynch syndrome, but your children will have a 50% chance of inheriting the alteration.
Genetic testing for Lynch syndrome
Genetic testing for Lynch syndrome will involve having a blood test. DNA will be extracted from your blood to look for genetic changes (or variants) that cause disease or increase your risk of developing a disease. This testing takes approximately 3 months to complete.
Genetic testing for Lynch syndrome helps us to understand you and your family’s risk of developing cancer in the future. Positive test results will also help our doctors to understand the treatments you may require. They will use it to develop an enhanced cancer prevention programme just for you. If you have cancer, you will be eligible for therapies that know work best for people with Lynch syndrome such as immunotherapy.
Having genetic testing is optional. Your decision will not affect the standard of care you receive. However, knowing you have Lynch syndrome will give you and your family access to personalised cancer prevention programmes, advice and treatments. It will also enable testing of other family members to ensure they are kept safe and reduce the chance of further cancers developing in the family.
If you would like to find out more about genetic testing follow this link that will help you understand the 3 possible outcomes of genetic testing (Link to website section about genetic testing)
What does it mean when my doctor or nurse talk about cancer in the general population?
Unfortunately, cancer is common, and in the majority of cases is not inherited. As many as 1 in 2 people will develop cancer in their lifetime. That is 50% of the world’s population.
Most cancers are not inherited and occur out sporadically or out of the blue. Their origin is based on the tumour cells itself. Some common reasons for cancer are aging, exposure to chemicals, radiation, hormones or other factors in the body or environment. Sporadic cancers usually occur at a later age in life because people are not born with a predisposition, and the development of cancer usually takes many years to generate.
It’s important to be aware of this because nobody is free from cancer risk, and when clinicians explain to people with inherited cancer predisposition syndromes that they have an increased likelihood to develop certain cancer types, they make comparisons to the general population, so it is helpful to know that everyone is at risk to some extent. If you are reading this, and you don’t have an inherited cancer predisposition syndrome, it is important to still take steps to prevent cancer from occurring. For instance, take part in national cancer prevention programs such as the National Bowel Cancer Screening program or the National Cervical Cancer Screening Program.
Will I develop cancer?
The risk or likelihood to develop cancer is there, even in the general population. Lynch syndrome make certain cancer types (not all) more likely to happen. This is due having less protection from the cancer mismatch repair genes. This doesn’t mean that you will develop cancer for sure. But having less protection makes it more likely.
However, there is a way in which you can balance out this increase likelihood, and that is by taking control and remain vigilant. If you have a new concerning symptom that last for over 2 weeks, we recommend that you seek medical advice. In addition, we recommend that you take control of your personalised surveillance program, and in addition to that, follow a healthy lifestyle that will help you to reduce, and balance out, this increased likelihood to develop cancer, or at least catch it and treat it early. If you have been diagnosed with Lynch syndrome, you can find your personalised recommendations in the screening & risk reducing strategies section.
Not everyone living with Lynch syndrome will develop cancer. The likelihood to develop cancer is considerably lower in individuals who know that they have Lynch syndrome and follow their enhanced screening programme, compared to individuals who are unaware of their diagnosis. This is because knowing about the risk gives individuals the chance to take action in a timely manner, and this helps to ensure that cancer is detected at an early stage so it can be treated more effectively.
It is important to highlight that Lynch syndrome is a late onset cancer susceptibility syndrome, and it doesn’t usually affect children. This is why cancer prevention programs starts between the ages of 25 to 35. The start age of your family cancer prevention programme will depend on which gene is implicated. For instance, individuals with genetic changes in the PMS2 gene have a lower likelihood of developing cancer compared to those who have a genetic change in the MLH1 gene. However, what really makes a difference is to follow your personalised screening programme, and make sure you make the most of your regular check-ups. In any case, if you have a family history of earlier onset of cancers, let your clinician aware, as you and your family might begin screening a little earlier.
It is impossible to know your exact risk or likelihood to develop cancer due to Lynch syndrome because other factors influence the risks such as lifestyle, the foods you eat, and environmental toxins. The way Lynch syndrome behaves in you and your family can be very different as the affected Lynch syndrome genes interact with other genes as well. Family history should be taken into consideration, but each family member will be affected differently.
As you are aware, there is a risk of cancer even in the general population. What is important is that you remain vigilant. If you have a new concerning symptom that last for over 2 weeks, we recommend that you seek medical advice.
There are other general lifestyle recommendations that will reduce your likelihood to develop cancer. You can find these lifestyle recommendations in the gene-specific information in the screening & risk reducing strategies section.
What does my genetic test result mean?
After approximately 3 months you will be given your genetic result. You have been waiting for this and these 3 months, which might feel like a long time. Now that you have spoken to your team and have your results, you might have some questions. Please, read on the information below as many times as you need so you can understand your results and its implications to you and your family. And most importantly, what can you do to reduce your prevent cancer and balance out the risk.
The main concern in Lynch syndrome is colorectal cancer. For women endometrial (womb) cancer is also a concern, and to a lesser degree ovarian cancer. There is small increase in likelihood to develop few other cancers. These other cancers are: pancreatic, kidney, urinary tract, skin, brain, and other gastrointestinal cancers. However, these other cancers are seen occasionally, and the risk is small, and generally is less than a 5% increase if you compare this risk to rest of the general population.
The risk or likelihood of developing cancer depends on 3 factors: which gene is implicated, gender, and age.
Age: The likelihood to develop cancer is very low at early age. This is the reason why bowel screening doesn’t start till the age of 25-35. The likelihood of developing cancer increases with age, the same as in the rest of the population.
Gender: Men tend to have a higher risk of developing colorectal cancer as compare to Women. However, women have the additional risk of endometrial and ovarian cancer.
Gene: Different genes have a different likelihood to develop cancer. There are some websites that can give you percentages of risk. It can be difficult to look at graphs and make sense of the information, especially when the information personal to us. We recommend that you have a look at this information with a health care professional who can personalise the information for you and can answer your questions appropriately. However, if this is something that you would like to look at, you can visit this website:
Is there a cure?
There is no cure for Lynch syndrome, but your clinicians will help you put together a personalised screening programme that will help you manage Lynch syndrome so you can balance out your increase risk of cancer and live a normal life.
I have Lynch syndrome and I have already have cancer. Can I get cancer again?
Yes, cancer can happen again. This is why is important to follow your personalised cancer prevention program, as this will significantly reduce your risk of cancer, or catch it and treat it early.
Screening & risk reducing strategies:
General recommendations for Lynch syndrome
Genetic results & recommendations
The next section will give you your general screening and lifestyle recommendations according to your genetic result. We have developed a gender, age, and genetic result tool that will give you personalised recommendations just for you. So the information is clear, you know what to do at your age, and most importantly, you do not need to work this out yourself:
Tool currently under construction – For now follow the personalised recommendations given to you by your clinician
Useful links:
Lynch Syndrome UK
Macmillan Cancer Support
Telephone support line on 0808 808 00 00 Monday-Friday, 9am-8pm, www.macmillan.org.uk
Bowel cancer UK